ISN Academy: Hemodialysis
Is hemodialfiltration a step ahead? No convincing improvement in physical activity
Effect of hemodiafiltration on measured physical activity: primary results of the HDFIT randomized controlled trial
Pecoits-Filho et al. Nephrol Dial Transplant. 2021;36(6):1057-70
Summary: 195 hemodialysis (HD) patients were randomised to high-volume hemodiafiltration (HDF) or high-flux haemodialysis for 6 months, with assessment of physical activity via an accelerometer worn for 24 hours after dialysis at baseline, 3 months and 6 months. There was no significant increase in step count with HDF at 3 months or 6 months (538 more steps with HDF/24h overall, 95%CI -330 to 1407 steps/24h). There were no significant improvements in physical activity in any portion of the 24-hour post-dialysis period, and there were no differences in quality of life scores.
Comment: The research team hypothesised that improving clearance of middle-molecular weight toxins with HDF may improve physical activity, in keeping with trials which have shown HDF benefits for patient-reported outcomes such as health-related patient satisfaction. Unfortunately, no such advantage has been demonstrated. It is possible that the study is underpowered to identify a smaller effect size. Other trials have demonstrated cardiovascular and mortality benefits from very modest improvements in physical activity, and it is difficult to define what improvement in physical activity would be considered clinically meaningful. Further studies may be needed to examine for a smaller effect size and for improvements in long-term patient outcomes.
ISN Academy: Transplant
Does azathioprine still have a place as first line immunosuppression for kidney transplantion?
Mycophenolate mofetil versus azathioprine in kidney transplant recipients on steroid-free, low-dose cyclosporine immunosuppression (ATHENA): A pragmatic randomized trial
Ruggenenti et al. PLoS Med 18(6): e1003668.
Summary: 233 adult recipients of their first deceased donor renal transplants, receiving low-dose thymoglobulin and basiliximab induction were randomised to either azathioprine 75-125mg daily (n=114) or mycophenolate 750mg BD (n=119), in conjunction with cyclosporine (microemulsion formulation, eg. Neoral) without steroids, with a median follow-up of 4 years. Biopsy proven chronic allograft nephropathy (CAN) was seen in 29 of 87 (33%) on MMF and 31 of 88 (35%) on AZA (P=0.69). Biopsy proven acute cellular rejection was less common in the MMF group, but this did not reach statistical significance (17% vs. 30%, HR 0.58, 95% CI 0.34 to 1.02, P=0.057).
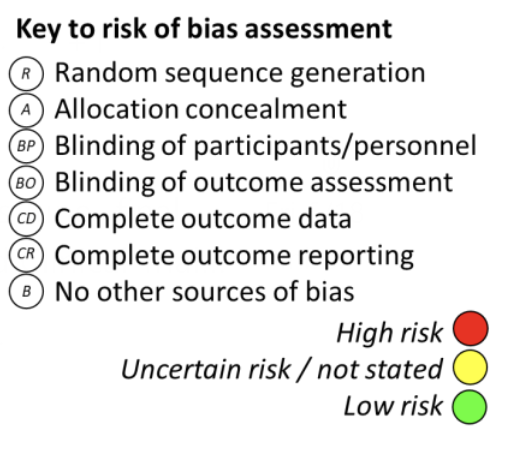
Comment: MMF, although more expensive, has replaced AZA as the standard antiproliferative used in kidney transplantation as it is associated with a lower rate of acute rejection in the first 6 months post-transplant. The authors of the present study hypothesised that early registration trials for MMF had overestimated its benefits as they were conducted with older formulations of cyclosporine. This unblinded randomised controlled trial utilised a regimen of immunosuppression therapy with low dose cyclosporine (a modern microemulsion formulation) and a steroid free maintenance to compare MMF and AZA. However, this trial found a concerning trend towards higher rates of acute rejection in the AZA treatment arm, albeit not quite reaching statistical significance. Further evidence would be required before concluding that AZA can replace MMF in low risk patients using a steroid free regimen.
ISN Academy: Acute Kidney Injury
Levosimendan increases renal blood flow in patients with AKI after cardiac surgery
Effects of levosimendan on renal blood flow and glomerular filtration in patients with acute kidney injury after cardiac surgery: a double blind, randomized placebo‑controlled study
Tholèn et al. Crit Care (2021) 25:207
Summary: In this single-center, double-blind, randomized controlled trial Tholen et al enrolled 29 hemodynamically stable patients with postoperative AKI after cardiac surgery without clinical indications for inotropic support. The patients were randomized to receive either levosimendan (12 μg/kg for 30 min followed by 0.1 μg/kg/min for 5 hours) or a placebo infusion. At inclusion, the mean serum creatinine was significantly higher, and the estimated GFR was significantly lower in the levosimendan group than in the control group. The increase in renal blood flow, measured using infusion clearance of para-aminohippuric acid, was significantly higher in the levosimendan group (15%) than in the control group (3%, p=0.011). Levosimendan also induced a more pronounced decrease in the renal vascular resistance than placebo (-18% vs -4%, respectively, p=0.043). However, the difference in the GFR, measured using infusion-clearance technique, did not reach statistical significance.
Comment: AKI is a common complication after cardiac surgery, associated with poor outcome. This is the first study that investigated the potential effect of levosimendan on renal blood flow and GFR in patients with post-operative AKI who did not require inotropic support. Interestingly the study demonstrated a significant increase in the renal blood flow, but no significant improvement in GFR. This is consistent with multiple larger RCTs in cardiac surgery patients where analysis of secondary endpoints revealed no evidence that levosimendan improved renal outcomes. There are several limitations that complicate the interpretation of the results, including low number of patients and significant differences in the initial characteristics of the groups. Currently, there is no evidence to recommend levosimendan for the treatment of AKI.
ISN Academy: Hemodialysis
Tenapanor add-on for hyperphosphatemia in hemodialysis patients: a phase II randomized clinical trial
Therapeutic effects of add-On tenapanor for hemodialysis patients with refractory hyperphosphatemia
Shigematsu et al. Am J Nephrol. 2021 Jun 7;1-11
Summary: Fourty-seven hemodialysis patients were randomized to receive either tenapanor (n=23) or placebo (n=24). Patients in the intervention arm received 30mg twice daily tenapanor shortly before meals with dose reduction to side effects. During the six-week study period, mean serum phosphorous changed from 6.77mg/dL to 4.67 mg/dL in the tenapanor arm, compared to 7.01mg/dL to 6.69mg/dL in the placebo arm. There was a between-group difference of -2.07mg/dL (p < 0.001). Target achievement of serum phosphorus (≤6.0mg/dL) at week six was 87.0% in the tenapanor group. Adverse events were higher in the tenapanor arm (18/23, [78.3%]) compared to placebo (9/24 [37.5%]) with the most frequent side effect gastrointestinal-related (16/23 [69.6%]). Half of the patients in the tenapanor group required dose reduction due to the development of diarrhoea.
Comment: Tenapanor is a novel inhibitor of the Na+/H+ antiporter which results in reduced paracellular phosphate transport in the gastrointestinal lumen, in a mechanism of action differing from currently available phosphate binders. This was a pragmatic phase II multicentre, double-blinded trial. Tenapanor was effective in lowering serum phosphorous over the six-week study period. This came at the expense of the commonly reported side effect of diarrhoea, which may be particularly poorly tolerated in the haemodialysis population. Future studies are required to assess the long term safety and tolerability of this novel agent and could include a dose-incrementing regimen to reduce side-effects.
ISN Academy: Transplant
Tocilizumab induces favourable changes in transplant kidney recipient T-cell populations
Interleukin-6 blockade with tocilizumab increases Tregs and reduces T effector cytokines in renal graft inflammation: A randomized controlled trial
Chandran et al., Am J Transplant (2021) 21(7) doi: 10.1111/ajt.16459
Summary: 30 kidney transplant recipients with graft inflammation on surveillance biopsy within the first year post-transplant (Banff borderline change or Banff i or ti scores of 1-2 without tubulitis) were randomly assigned receive tocilizumab (TCZ) (monthly for 6 months) or no additional treatment. All patients continued standard immunosuppression regimens. After 6 months, there were no statistically significant differences in medians of Banff i-, t-, ti-scores, nor in the number of subjects with the resolution of borderline changes (9/16 vs. 8/16, p=0.99). A higher proportion of patients in the TCZ group had a decline in the ti-score (10/16 vs. 3/14, p = 0.03). When compared to controls, there was an increase in the proportion of Treg cells at months 3 and 6 in the TCZ full-dose group, along with a decrease in IFNγ-, IL-17-, and granzyme B producing CD4+ T cells. There were no cases of death or graft loss in the study. Three of 16 subjects discontinued TCZ prematurely (due to BK viremia, pneumonia/sepsis, and transplant pyelonephritis), and 4 of 16 subjects required reduced-dose TCZ due to cytopenias.
Comment: Many challenges remain in renal transplantation, with renal graft loss due to chronic immune-mediated injury being foremost. Use of biologics to target specific immune system pathways is attractive for many reasons, but aside from IL2 receptor antibodies, none have entered standard practice. Unfortunately, this study failed to demonstrate a clear benefit, without clear histological evidence of regression of inflammation due to TCZ. However, given its small size, and failure to reach target recruitment, it still provides useful information to inform further studies. In particular, the changes in immune markers, including an increase in Treg cells and decrease in potentially immunoreactive subtypes of CD4+ T cells, suggests a more graft tolerant immunological milieu. Interestingly, a phase 3 RCT (NCT04561986) exploring TCZ vs standard care in chronic antibody-mediated rejection was recently registered – so watch this space…
ISN Academy: Hypertension
A MINT-Y fresh approach to blood pressure control
Effectiveness of motivational interviewing on medication adherence among Palestinian hypertensive patients: a clustered randomized controlled trial
Khadoura et al. European Jouran of Cardiovascular Nursing (2021) 20,411-420
Summary: Three hundred and fifty-five self-identified treatment non-adherent individuals with hypertension requiring at least one antihypertensive medication were randomised to either three motivational interviewing (MINT) sessions to improve adherence to prescribed antihypertensives or standard care. Adherence in those undergoing MINT versus standard of care was markedly greater (OR=6.28;95% CI:3.20-12.33; P<0.001). Moreover, MINT subjects had a mean drop in systolic blood pressure (BP) of 4.5mmHg (OR=0.18, 95% CI: 0.06-0.55; P=0.002); and 3.24mmHg drop in diastolic BP (OR=0.26: 95% CI:0.09-0.76; P=0.013). Participants also reported significant improvement in intrinsic motivation and self-efficacy following these sessions.
Comment: Efficacy of pharmacotherapies are significantly limited in hypertension by treatment nonadherence, thus the importance of strategies to improve compliance. MINT appears to have been a highly successful tool in hypertensive patients living in Gaza. The major limitation of this study is its dependence on self-identification and assessment of adherence by participants with no surrogate validation such as drug level monitoring or pill counting. Other consideration impacting on results include uneven randomisation of number of antihypertensives and frequency of hypertensive therapies between arms. Follow up was also short (one month) and thus the legacy effect of this brief intervention on chronic disease management is unknown. Large scale studies of this class of intervention are lacking, but could conceivably have an important impact on patient outcomes.
ISN Academy: Acute Kidney Injury
Restriction of intravenous rehydration in ICU patients?
Restrictive fluid management versus usual care in acute kidney injury (REVERSE-AKI): a pilot randomized controlled feasibility trial
Vaara et al. Intensive Care Med (2021) 47:665-673
Summary: This multi-centre pilot study randomised 100 critically unwell patients with AKI to restrictive fluid management (RFM) or local usual care. The primary aim was to assess whether RFM results in a difference in cumulative fluid balance at 24 hours without causing serious harm. The RFM regimen consists of a series of recommendations to reduce total fluid input and aim for a negative cumulative fluid balance (using RRT if necessary). Only the statistician conducting data analysis was blinded to treatment allocation due to the study design. Mean cumulative fluid balance at 72 hours was –1080ml in the RFM arm and +61ml in the usual care arm (p = 0.033). There was no statistically significant difference in AKI duration between the two arms. Fewer patients experienced adverse events in the RFM arm compared to the usual care arm (22.4% vs 49%, p = 0.001). RFM was associated with fewer patients receiving renal replacement therapy compared to the usual care regime (13% vs 30%, p = 0.043).
Comment: Avoidance of iatrogenic fluid overload is important given the potential implications for patient morbidity and mortality. This feasibility trial focussed on the safety of restrictive fluid management in critically unwell patients with AKI. It is reassuring that restrictive fluid management reduced the cumulative fluid balance and number of adverse events without prolonging AKI duration. The main limitation of the study was the lack of standardisation in practice between different centres for both the intervention and control arms. This was demonstrated by the high number of protocol variations (36.7% in the RFM arm and 9.8% in the usual care arm) with 18.4% related to excess maintenance fluid in the RFM arm. Unfortunately, the extent of excess fluid maintenance was not reported by the authors. Furthermore, the study design did not permit blinding of the study participants or personnel representing a potential for significant bias. Overall, this pilot study has demonstrated that restrictive fluid management can be undertaken without serious harm so will hopefully lead to a full trial.