ISN Academy: Acute Kidney Injury
Can acute kidney injury be prevented?
Can acute kidney injury be prevented?
Teprasiran, a small interfering RNA, for the prevention of acute kidney injury in high-risk patients undergoing cardiac surgery
Thielman et al. Circulation 2021. DOI: 10.1161/CIRCULATIONAHA.120.053029
Summary: 360 patients undergoing elective cardiac surgery, with at least 1 risk factor for acute kidney injury, were randomised to intravenous teprasiran (single bolus of 10mg/kg) or placebo. For patients undergoing cardiopulmonary bypass (99.7% of patients), treatment was given at 4 hours after discontinuation of bypass, while it was given after the last coronary anastomosis for patients undergoing off-pump surgery. There was a similar distribution of cardiac procedure types between groups, and similar intra-operative haemodynamic parameters. The teprasiran group had a 37% rate of AKI, defined by AKIN serum creatinine criteria, compared to 50% with placebo (odds ratio 0.58, 95%CI 0.37-0.92, p=0.02). There were lower rates of severe AKI and lower rates of AKI lasting 5 days or more. The benefit appeared consistent across age, cardiopulmonary bypass time, eGFR and diabetes status subgroups. At 90 days there was no difference in the composite outcome of death, renal replacement therapy or 25% reduction in eGFR. There were no concerning safety signals, including no increase in the risk of adverse effects that may relate to teprasiran therapy such as hypotension (1.2%) and elevated transaminases (<3%).
Comment: Cardiac surgery poses a high risk of acute kidney injury with associated morbidity, mortality and healthcare system costs. Teprasiran, as a synthetic small interfering RNA (siRNA), inhibits the DNA-binding transcription factor p53, which would otherwise mediate proximal tubular cell growth arrest or cell death in response to ischemia-reperfusion injury. The duration of the cellular effect is approximately 48-72 hours, which should avoid the long-term risk of malignancy potentiation. This is the first positive randomised controlled trial of a therapeutic agent to prevent or treat AKI. Progression to a phase 3 trial is underway, to examine the effects in a larger cohort and with further investigation of long-term efficacy and safety outcomes. Teprasiran is also being investigated for the prevention of delayed graft function in deceased donor kidney transplant recipients (NCT00802347 and NCT02610296).
ISN Academy: Transplant
Belatacept-based maintenance regime or continuation of calcineurin inhibitors?
Conversion from calcineurin inhbitor to belatacept-based maintenance immunosuppresion in renal transplant recipients: a randomized phase 3b trial
Budde et al. JASN 2021. DOI: 10.1681/ASN.2021050628
Summary: The efficacy and safety of converting stable kidney transplant recipients from maintenance calcineurinbased immunosuppression to belatacept was evaluated in this prospective randomised comparative trial. 446 participants were randomised, 1:1 ratio, to belatacept or calcineurin inhibitor (CNI). Similar 24-month graft survival rates were reported for both groups (belatacept 98% vs CNI continuation 97%; 95% CI OBF, -2.1 to 3.7). Sustained renal function improvement was documented in the belatacept conversion group (+ve slope 0.68ml/min/1.73m2) compared to the decline in the CNI continuation group (-ve slope -0.11ml/min/1.73m2). The 24-month mean adjusted eGFR was higher with belatacept conversion group than CNI control (55.5 vs 48.5 ml/min/1.73m2). There was a non-significantly greater risk of biopsy-proven acute rejection rate following belatacept conversion (HR 2.09, 95% CI, 0.94 to 4.65); although no greater incidence of dnDSAs when compared to the CNI group. Both groups had similar rates of serious adverse events, infections and discontinuations. Of note, there was one case of posttransplant lymphoproliferative disorder in the intervention arm.
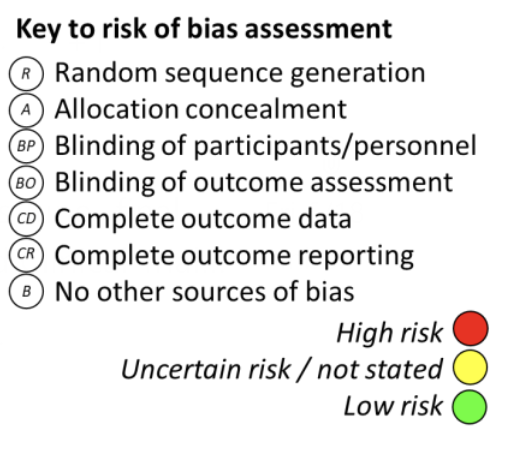
Comment: This prospective randomised study demonstrates comparable graft survival and an acceptable safety profile of belatacept compared to standard calcineurin inhibitor-based maintenance immunosuppression regimes. It contributes to the existing literature supporting belatacept as a viable alternative immunosuppression agent. The main weakness of this study was the lack of blinding of participants, study personnel and outcome assessors that may have influenced post randomisation behaviours, especially given biopsies for investigation of rejection were investigator-driven only, with no surveillance biopsies permitted. Future studies demonstrating long-term outcomes of belatacept infusion-based regimes should be performed to determine its place in transplantation care.
ISN Academy: End of Life Care
Tools for Advanced Care Planning in CKD patients
Advanced Care Planning Coaching in CKD Clinics: A Pragmatic Randomised Controlled Trial
Lupu et al. AJKD 2021. DOI: 10.1053/j.ajkd.2021.08.019
Summary: This multicentre, unblinded, randomised controlled trial randomised 264 participants aged 55 years and above, with stage 3-5 chronic kidney disease. Individuals were given the same educational material regarding advanced care planning (ACP) and assigned either 60 minutes of in-person coaching by nurses or social workers with experience in palliative care plus follow up phone calls monthly or asked to review ACP material on their own (enhanced standard care). Measurement of the primary outcomes approximately 4 months post intervention included scoring on a 45-point ACP engagement scale and medical record documentation of an advanced care directive (ACD). The patients who received the intervention overall scored 1.9 points higher in the ACP engagement scale (β = 1.87, 95% CI 0.13-3.64), and when adjusted for clinic site, were 79% more likely to have an ACD (RR 1.79, 95% CI 1.18-2.72). One of the three sites was responsible for the majority of the overall difference in ACD (Phomogeneity=0.04). Four of the intervention group patients were noted to experience moderate emotional distress during the study
Comment: Advanced care planning is an invaluable discussion particularly with the chronic kidney disease patient cohort who have a high burden of medical comorbidities, and particularly prior to the initiation of dialysis where illness and fatigue can often overwhelm a patient’s ability to make complex decisions. This pragmatic study showed significant increase in ACD documentation in the coached group and a high level of patient satisfaction with the intervention with 77.9% reporting it encouraged them to seek more information about ACP. It is notable that the effect seemed to be driven almost entirely by one of the three sites, emphasising the importance of site factors with interventions such as this. The limitations of this study include that non-English speaking patients were excluded, and that approximately 30% of engagement scales were missing. In addition, high variability in coaching session time and follow up frequency likely highlights the challenge of managing a highly individual discussion with patients. This area needs more research to guide clinicians in effective strategies to engage patients and translate these discussions into clear ACD.
ISN Academy: Anemia, Iron and Trace elements
Higher single dose, but less frequent iron supplementation in prevalent haemodialysis patients
Comparison of iron dosing strategies in patients undergoing long-term haemodialysis: a randomised control trial
Bielesz et al. Clin J Am Soc Nephrol;16(10):1512-1521
Summary: In this prospective, randomized, open-label non-inferiority trial, higher single doses of ferric carboxymaltose (FCM) (intervention) were compared to higher-frequency schedule of lower doses of iron sucrose (IS) (control) in chronic haemodialysis patients. Seventy-one participants were randomized to receive IS at a fixed dose of 100mg every two weeks (continuous dosing) and 70 patients received FCM at a fixed dose of 500mg every 10 weeks (periodic dosing). Both treatment arms received equal cumulative 2-g doses of intravenous iron over the total 40-week study period. At week 40, haemoglobin was lower in the periodic dosing arm (mean difference -0.47g/dl, 95% CI, -0.95 to 0.01; p = 0.09 for noninferiority [at a margin of 0.8g/dL]), with a similar finding in the modified intention-to-treat analysis. Infection rates were significantly higher in the IS arm (n = 39, 55%) compared to FCM (n = 16, 23%), although there was no overall difference in serious adverse events (41% and 39%, respectively).
Comment: Periodic dosing of FCM did not meet the non-inferiority margin compared to continuous dosing of IS in this study. Strengths of this study include its pragmatic design and the head-to-head comparison of two iron formulations. Several factors, such as high dropout rates and out-of-protocol modifications in ESA and iron therapy at the discretion of the attending physician, complicate interpretation of these results. Reasons for the higher infection rates in the IS arm were not clear. The authors speculated that the slightly higher prevalence of diabetes and dialysis catheters in the IS arm might have played a role. In summary, the choice between the two iron preparations is a balance of efficacy, cost and safety profile. Further head-to-head randomized trials comparing various iron preparations over more diversified study populations will assist in clarifying non-inferiority between products and regimens.
ISN Academy: Glomerular Diseases
The best-laid schemes of mice and men for anti-CD20 therapies in paediatric nephrotic syndrome
Human or chimeric monoclonal anti-CD20 antibodies for children with nephrotic syndrome: a superiority randomized trial
Ravani et al. JASN 2021. DOI: 10.1681/ASN.2021040561
Summary: One hundred and forty participants aged 2-24 years with steroid- and calcineurin inhibitor (CNI)- dependent nephrotic syndrome were randomised to either ofatumumab or rituximab. All participants were in remission at point of randomisation and weaning of steroids and CNIs were the same in both arms. 52.8% of the ofatumumab arm and 51.4% of the rituximab had reached the primary endpoint of relapse within 12 months (OR 1.06; 95% CI0.55 to 2.06). 75.7% in the ofatumumab arm and 65.7% had relapsed by the end of 24 months follow up (OR 1.6; 95% CI 0.8 to 3.3). There were no major adverse events in either treatment arm.
Comment: Complete remission from paediatric nephrotic syndrome is an important target to reduce the iatrogenic risks of long term steroid and CNI exposure, especially from a metabolic perspective. This Genoise study failed to demonstrate a benefit of fully human anti-CD20 ofatumumab over chimeric human/murine rituximab for childhood nephrotic syndrome in those high risk for relapse. Both appeared to have similar safety profiles, and despite an extended binding site and higher CD-20 affinity, ofatumumab did not result in any longer periods of B cell depletion than rituximab. This single centre study will hopefully inform pooled analyses to help determine clinical superiority between these two therapies in future systematic reviews. For now, it appears that older, potentially more economical therapies are just as effective in childhood nephrotic syndrome.
ISN Academy: Diabetes
Colchicine does not prevent overt nephropathy in patients with early diabetic kidney disease
Low-dose colchicine in type 2 diabetes with microalbuminauria: a double-blind randomized clinical trial
Wang et al. J. Diabetes 2021 DOI: 10.1111/1753-0407.13174
Summary: In this double-blind, placebo-controlled trial 160 patients with type 2 diabetes and urinary albumin-tocreatinine ratio (uACR) 30 to 300 mg/g were randomized to either colchicine 0.5 mg/day or placebo. All patients received ACE inhibitors or angiotensin receptor blockers for at least 3 months before enrolment. Over 36 months of follow up, the primary end-point of transition to overt nephropathy (uACR >300 mg/g) was registered in 51.4% patients in the colchicine group and in 54.1% patients in the placebo group (HR 1.07, 95% CI 0.68 to 1.67, p = 0.78). None of the patients developed doubling of serum creatinine, the need for renal replacement therapy or died of renal disease, and there were no significant differences in eGFR or uACR. However, the levels of markers of neutrophil-related chronic inflammation (NRCI), including C-reactive protein levels, neutrophil counts and neutrophil-to-lymphocyte ratio, were significantly lower in the colchicine group (all p < 0.05). The rates of adverse events were similar in both groups.
Comment: Type 2 diabetes mellitus is one of the most common causes of CKD worldwide. Previous clinical and experimental studies demonstrated strong associations between NRCI and diabetic kidney disease (DKD) occurrence and progression. However, this RCT showed that continuous NRCI suppression with colchicine does not prevent the progression of early DKD to overt nephropathy. The limitations of the study include relatively small sample-size and short follow-up, that could prevent the detection of long-term outcomes in both groups. In conclusion, the results of the trial do not support the use of colchicine in the treatment of early DKD.