10 Recommendations for Global Kidney Health
- Work toward prevention, early diagnosis, treatment and management of kidney diseases.
Managing risk factors can help to keep healthy kidneys, as well as to slow down the progression of already developed diseases. In order to prevent and manage AKI and CKD in adults and children, public health policies need to be developed which have to:
- Ensure healthy adult, maternal and child lifestyles and nutrition.
- Reduce the burden of co-occurring conditions such as diabetes, hypertension, cardiovascular diseases and/or obesity.
- Reduce unhealthy addictions burden from drugs, tobacco, and/or alcohol.
- Promote safe work environments and assist in situations that threaten safety and/or security (such as natural hazards or violence). Strategies that include medications, kidney replacement therapy (KRT), promote recovery and prevent recurrence need to be created.
- Prevent and respond to epidemic and endemic infectious diseases that impact kidney health.
- Monitor the burden of kidney diseases.
To better understand the burden of AKI and CKD data is needed, therefore:
- surveillance programs need to be implemented and supported to better understand the global burden of AKI and CKD within and outside the context of non-communicable diseases.
- robust national and regional registries on the incidence, prevalence and aetiology of AKI, CKD, and kidney failure with or without KRT need to be developed.
- Raise public awareness of kidney diseases.
Improved health literacy among patients on kidney disease and its risk factors would empower patients in decision-making and self-management of their conditions. Understanding the association of kidney disease with other non-communicable diseases as well as the risk factors that may lead to developing kidney needs to be deepened. This could be achieved through multiple approaches such as informational campaigns paired with primary care, and community health centres.
- Address kidney diseases across the life course through universal health coverage.
Universal health coverage (UHC) ensures that all individuals receive quality health services, from health promotion to rehabilitation, from treatment to palliative care, depending on their needs and without financial burden throughout their life-course. For optimal kidney health, this begins with universal access to antenatal care and child health visits, and permits sustainable access to effective and affordable quality diagnostics and medications for detecting and treating risk factors, such as hypertension, diabetes, cardiovascular and urologic diseases. This helps to delay kidney disease progression.
- Integrate kidney disease services within existing health and multisectoral initiatives.
There is a need for a stronger push to ensure integration and synergies for kidney disease prevention and treatment within existing health and multisectoral initiatives. Policies should be developed and implemented to serve as the needed push. They should be developed following the current frameworks promoted by the World Health Organization and the United Nations such as:
- 2030 Agenda for Sustainable Development.
- Prioritisation of Universal Health Coverage.
- Life Course approach to chronic diseases.
- United Nations-wide call from Secretary-General António Guterres “to use the recovery to build back better” for non-communicable diseases.
- Close education gaps on kidney diseases among all healthcare workers.
Knowledge of kidney disease needs to be deepened among healthcare workers at all levels. This ensures that a lack of clinical awareness does not become a barrier for patients to get appropriate access to essential tools and medications required for protection, diagnosis, and treatment to prevent kidney injury and failure.
- Invest in strengthening the kidney care workforce.
Supporting education and the growth of a skilled nephrology workforce is needed to ensure the highest level of patient care across the spectrum of kidney diseases. The nephrology workforce needs to be confident when implementing screening, prevention, and treatment of kidney disease from its early acute stage to its chronic stages. This includes using kidney replacement therapy, conservative management and palliative care.
- Strive towards equitable and sustainable access to care for kidney failure.
Develop and implement policies that ensure equitable access to kidney disease care for all, regardless of gender, income or ethnicity. Everyone needs to have access to:
- Early diagnosis of kidney disease.
- Appropriate treatment.
- Kidney replacement therapies and transplantation.
Additionally, safe, ethical, affordable, and sustainable programs that are appropriate to each region’s cultural, religious, and social context need to be supported. Programs should incorporate quality metrics and processes to ensure accountability.
- Promote and expand kidney transplantation programs.
Transplantation programs need to be promoted and expanded across the globe. These programs must equal access to transplantation regardless of an individual’s income and uphold ethical practice in management of all donors and recipients. The integration of such programs must be respectful, recognising each region’s cultural characteristics. Adherence to the principles of the Declaration of Istanbul should be universal. Programs should incorporate quality metrics and processes to ensure accountability.
- Support research for kidney diseases.
Local, regional, and collaborative international research in acute kidney injury (AKI) and chronic kidney disease (CKD) needs to be supported. This would deepen understanding of kidney disease, which would eventually lead to better prevention and treatment strategies. Ethical principles in the conduct of research are critical. For advancing in this field:
- Publishing research work in mainstream journals needs to be promoted and facilitated.
- To advance the research and treatment of kidney diseases, human resources in the academic and medical workforce must be increased and supported.
News
ISN Advocacy Newsletter – Bridging the Gaps – July 2024
Bridging the Gaps: Update on the ISN's Global Impact and Leadership in Kidney Health Advocacy Dear members and allies, Welcome to the latest edition of Bridging the Gaps, your go-to source for updates on ISN global kidney health advocacy initiatives. This quarterly newsletter brings you the most significant developments and successes in our collective efforts to...
Help Combat Organ Trafficking: Support the DICG’s Campaign for World Day Against Trafficking in Persons
The Declaration of Istanbul Custodian Group (DICG) has launched a campaign to participate in the United Nations Office on Drugs and Crime’s World Day Against Trafficking in Persons, held on July 30. Access DICG resources on organ trafficking here The DICG’s theme for the campaign is “Recognizing Red Flags for Organ Trafficking,” highlighting warning signs that...
Hear From Global Experts on Equitable Access to Innovative Therapies
Aligning with the 2024 World Kidney Day theme, "Advancing equitable access to care and optimal medication practice," Nature Reviews Nephrology has published an editorial on innovative therapies for diabetic kidney disease (DKD). Five global experts* from different world regions, including authors of the 2024 World Kidney Day scientific editorial, discuss barriers that must be...
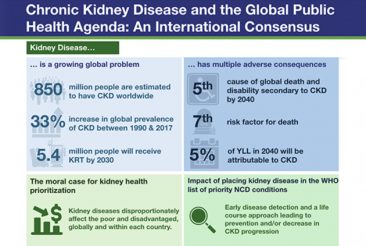
Positioning Kidney Disease at the Forefront of the Global Health Agenda: Use and Share Free ISN Resources
The ISN is committed to highlighting kidney health in the global health agenda and actively advocates with the World Health Organization to prioritize kidney health as a critical noncommunicable disease (NCD). Earlier this year, Nature Reviews Nephrology published “Chronic Kidney Disease and the Global Public Health Agenda: An International Consensus,” highlighting kidney disease as a...