ISN Academy: Chronic Kidney Disease
Unquenched: Aliskiren yet to find a place in CKD management
Direct Renin Inhibition in Non-diabetic chronic Kidney disease (DRINK): a prospective randomized trial
Tang et al. Nephrol Dial Transplant 2021. DOI: 10.1093/ndt/gfaa085
Summary: Seventy-six participants with stage 3-4 non-diabetic CKD were randomized to either aliskiren, a direct renin inhibitor (DRI), in addition to maximally tolerated angiotensin II receptor blocker (ARB) therapy, or ARB therapy alone. There was no difference in the annual change in eGFR between treatment arms (-1.67mL/min/1.73m2, 95% CI -1.99 to -1.36 in the aliskiren group vs. -1.53mL/min/1.73m2, 95% CI -1.85 to -1.20 in the control, p=0.52) over the 144-week follow-up period. The annual increase in the urine protein/creatinine ratio was statistically greater in the aliskiren arm (9.41mg/mmol, 95% CI 5.52 to 13.30 vs -1.68mg/mmol, 95% CI -7.23 to 3.87, p=0.002). There was no difference in the composite renal endpoint of doubling of baseline creatinine, 40% reduction of eGFR, ESKD or death. Nor was there any difference in cardiovascular morbidity or mortality. Hyperkalaemia was more common in the DRI+ARB arm.
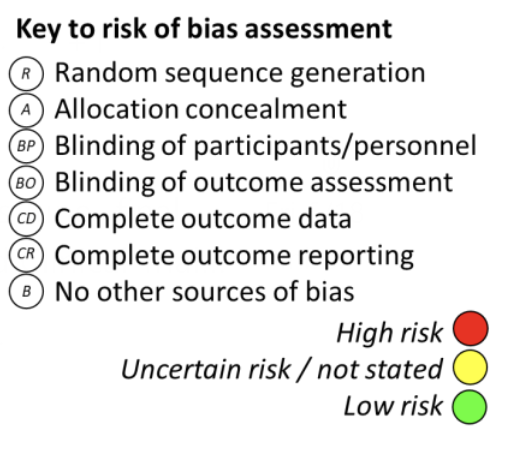
Comment: Aliskiren has been shown not to reduce decline in kidney function in people with diabetic kidney disease, although it did improve regression in albuminuria stage. The question of its potential role in renoprotection in other forms of CKD where renin-angiotensin system activation may play a role in pathogenesis was explored here. Authors were unable to demonstrate a renoprotective benefit for aliskiren, in particular no anti-proteinuric effects that had been seen in prior CKD trials. This relatively small trial found no signal of increased risk of cardiovascular death that was seen in earlier trials of the same drug in an older, predominantly Caucasian, diabetic population. This well conducted study with a long period of follow up provides important data for potential future meta-analyses exploring whether this agent has a role in targeted subgroups but does not support the addition of DRIs to current CKD management.
ISN Academy: Haemodialysis
No benefit of hemodiafiltration for neuropathy progression in a study conducted with FINESSE
Effect of Hemodiafiltration on the Progression of Neuropathy with Kidney Failure: A Randomized Controlled Trial
Kang et al. CJASN 2021. DOI: 10.2215/CJN.17151120
Summary: In the FINESSE trial, 124 hemodialysis patients were randomised to hemodiafiltration (HDF) or to continue hemodialysis for a mean of 41 months to assess progression of neuropathy scores. At baseline, 73% had neuropathy and 31% had moderate-to-severe neuropathy. After 48 months, the mean modified total neuropathy score (mTNS) in the hemodiafiltration group worsened by 1.7 points out of a possible score of 28 (standard error [SEM] 0.4), compared to a 1.2 point worsening (SEM 0.4) in the hemodialysis group. This difference was not significant (0.5 point, 95%CI -0.7 to 1.7, p=0.37), and nor were there any differences within subgroups. There was no survival benefit or difference in adverse effects. The convection volumes with HDF were satisfactory with a median volume of 24.7L (interquartile range 22.4-26.5L).
Comment: Uremic neuropathy is a common complication of chronic kidney disease and is associated with disability and poor quality of life. While the pathophysiology remains poorly understood, HDF offered a promising benefit by improving clearance of middle molecules which may be implicated in nerve dysfunction. Unfortunately, no such benefit has been demonstrated. There was significant loss to follow-up (51% of participants) due to death, transplantation, dialysis unit transfer or withdrawal. Although this may have reduced the study’s ability to demonstrate a treatment effect, including in subgroups such as those without co-morbid diabetes, the narrow confidence interval of the results suggests that haemodiafiltration is unlikely to result in a clinically meaningful improvement in mTNS scores, defined as an improvement of at least 2 points. The search for disease-altering therapy for uremic neuropathy continues.
ISN Academy: Transplant
Is belatacept the BEST way to avoid calcineurin inhibitors and steroids in patients with kidney transplant?
Belatacept for Simultaneous Calcineurin Inhibitor and Chronic Corticosteroid Immunosuppression Avoidance Two-Year Results of a Prospective, Randomized Multicenter Trial
Kaufman et al. CJASN 2021. DOI : 10.2215/CJN.13100820
Summary: This study provides 2-year follow-up of the BEST trial, where 333 patients were allocated into two belatacept study groups without a calcineurin inhibitor (belatacept/alemtuzumab and belatacept/anti-thymocyte globulin [rATG]) and one control group (tacrolimus/rATG) in 1:1:1 ratio prior to kidney transplantation. Patients in all groups received mycophenolate and a short (5 day) course of steroids. The primary outcome was the composite of patient and renal survival or eGFR of <45mL/min/1.73m2 measured at 2 years of follow-up. The outcome occurred less often with belatacept/alemtuzumab (10%) and belatacept/rATG (13%) than with the control group (21%) but this was not statistically significant (p=0.99 and p=0.66). Patient and graft survival rates were similar. For both belatacept-based regimes, the incidence of eGFR falling to <45mL/min/1.73m2 at 2 years posttransplant was lower (8% and 8%) than for tacrolimus-based group (19%, p=0.04 and p=0.05). The rate of acute cellular rejection was higher in both belatacept groups (19% and 25% compared with 7%). The incidence of serious adverse effects was similar in the study and control groups, but the rate of neurotoxicity and gastrointestinal adverse events was lower in the belatacept-based regimens.
Comment: Belatacept, which blocks CD28-mediated T-cell costimulation, was approved by the FDA after the results of BENEFIT and BENEFIT-EXT trials, which used cyclosporine in the control treatment and in which steroids were not withdrawn. This study suggests that medium-term outcomes with belatacept are similar to tacrolimus when either is used with lymphocyte depleting induction and mycophenolate, and with early steroid withdrawal. The higher rates of acute rejection in the belatacept-based arms were comparable to those seen in the earlier studies, and it is notable that long-term follow up of these trials found superior graft outcomes with belatacept. A current study, comparing belatacept/everolimus/early withdrawal of steroids with belatacept/mycophenolate/chronic steroids, after rATG induction (NCT04849533) is recruiting.
ISN Academy: Nutrition and Hydration
Salt substitute reduces rates of stroke, cardiovascular events and death
Effect of Salt Substitution on Cardiovascular Events and Death
Pitt el al. NEJM 2021. DOI: 10.1056/NEJMoa2110956
Summary: 20,995 participants who had history of stroke, or who were 60 years or older with hypertension, were recruited from 600 rural villages in five provinces across China and enrolled in an open-label, cluster randomised trial. Villages were supplied with either a reduced sodium salt substitute (75% NaCl with 25% KCl) or regular salt (100% NaCl) for use in their cooking. Mean duration of follow up was 4.74 years. The primary end point of stroke was lower in the salt substitute group (absolute difference, 4.51 events per 1000 person-years; rate ratio, 0.86 [95% CI, 0.77 to 0.96]; P = 0.006). The secondary composite endpoint of major cardiovascular events was also significantly lower in the salt substitute group (absolute difference, 7.2 events per 1000 person-years; rate ratio, 0.87 [95% CI, 0.80 to 0.94]; P <0.001), as was death from any cause (absolute difference 5.33 events per 1000 person-years; rate ratio 0.88 [95% CI, 0.82 to 0.85]; P <0.001). Of note, the salt substitute reduced systolic blood pressure by a mean difference of 3.34mmHg (95% CI, -4.51 to -2.18). Importantly, there was no difference in serious adverse events related to hyperkalaemia or sudden cardiac death.
Comment: This was an enormous study with an interesting design. Villages in rural China were recruited to be randomized, then individuals with risk factors for cardiovascular disease were sampled from within each village who could then be followed to ascertain the study endpoints. Given the rising burden of cardiovascular diseases in low- and middle-income countries, this low-cost intervention seems a great measure to protect the health of vulnerable populations. The treatment effect may be reduced by some crossover in salt and salt substitute use, including access to regular salt with meals outside the home. The generalizability of the study is reduced by the single ethnicity of the participants and the high baseline salt use of 20g per person per day.
ISN Academy: Paediatric Nephrology
A self-management program might improve knowledge, behaviors and quality of life among adolescents with chronic kidney disease
Self-Management Program for Adolescents with Chronic Kidney Disease: A Randomized Controlled Trial
Sezer et al. J Ren Care 2021. DOI: 10.1111/jorc.12357
Summary: Forty adolescent participants (aged 12-21) with stage 3-4 CKD or dialysis dependence, and their families, were randomized to a self-management program or standard care. The intervention involved 3 sessions providing CKD information and advice on self-management, and a series of 6 fortnightly home visits to monitor clinical outcomes and provide re-education if needed. After 3 months, participants completed a Self-Management Assessment form and Paediatric Quality of Life Inventory-Adolescent Form. There was overall improvement in self-management knowledge and behaviors, in the Paediatric Quality of Life score, and in anxiety scores (p all < 0.05), but not in self-efficacy. There were no significant improvements in GFR, albumin, creatinine, or haemoglobin levels.
Comment: Adolescents with chronic kidney disease face a significant treatment burden with a major impact on quality of life. Strategies to support self-management in adolescents with CKD are important in facilitating coping and adaptation. This study demonstrates promising progress with a resource-intensive self-management strategy. Further studies with larger numbers of patients, across a greater number of centres, and with longer-term follow-up, would help support the generalizability of the findings.