ISN Academy: Dialysis
Cooled enthusiasm for lower dialysate temperatures; no demonstrated benefit for cardiovascular outcomes
Personalised cooler dialysate for patients receiving maintenance haemodialysis (MyTEMP): a pragmatic, cluster-randomized trial
Garg et al, Lancet (2022).
Summary: MyTEMP study is a large pragmatic cluster-randomized trial, involving 84 hemodialysis sites and 15413 patients, testing the use of a personalized cooler dialysate temperature set at 0.5-0.9°C (32.9-33.6°F) below each patient’s body temperature measured at the start of each dialysis session, with a minimum temperature of 35.5°C (95.9°F) and a maximum of 36.5°C (97.7°F), compared to a standard dialysate temperature of 36.5°C (97.7°F). The intervention ran for more than 4 years and involved ~4.3 million hemodialysistreatments. The cooler dialysate group successfully achieved a lower dialysate temperature with a mean of 35.8°C (96.4°F) compared to 36.4°C (97.5°F). Approximately 80% of all patients were adherent to their center’s temperature assignment. During the trial duration, there was no difference in the primary outcome of the rates of cardiovascular death or hospital admission with myocardial infarction, ischemic stroke or congestive heart failure at 21.4% for the cooler dialysate group compared to 22.4% with the standard temperature group (adjusted hazard ratio 1.00, 95% confidence interval [CI] 0.89-1.11, p=0.93). There was no significant difference in the mean drop in intradialytic blood pressure or rates of intradialytic hypotension. Participants receiving cooler dialysate were 60% more likely to report feeling uncomfortably cold, according to systematic surveys conducted in 10 sites.
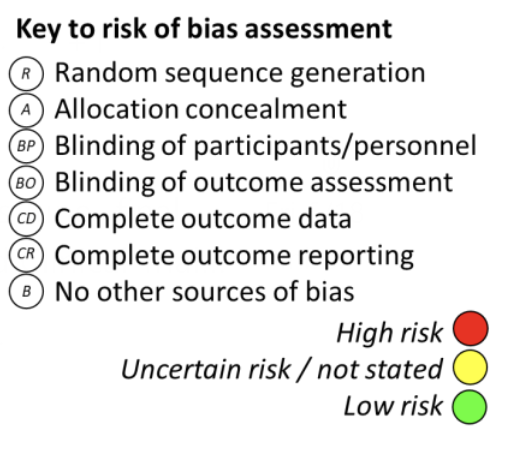
Comment: Several small studies and at least one meta-analysis have suggested a benefit of cooler dialysate to reduce intradialytic hypotension, and cohort studies have suggested a reduction in cardiovascular events with its use. Potential mechanisms include improved cardiac contractility, increased peripheral vascular resistance and reduced nitric oxide synthesis. In light of these findings, cooler dialysate has seen increasing use in clinical care. This very large and well-conducted study did not demonstrate a substantial cardiovascular benefit of this approach. It is possible that targeting a greater difference in dialysate temperature between the two groups might have been more likely to show a difference in outcomes, (e.g., comparing the personalized cooled dialysate to a set temperature of 37°C [98.6°F] as currently used in some units; thus, creating wider separation by which to test the hypothesis). Treatment was also not personalized to individual risk of intradialytic hypotension, which is the usual rationale for the treatment strategy in the first place, so the role of this individualization was not addressed. The study suggests The ISN-ACT (Advancing Clinical Trials) team presents this monthly round up of randomized trials in nephrology. Trials are selected not just for impact, but also to showcase the diversity of research produced by the global nephrology community. Each trial is reviewed in context and has a risk of bias assessment. We hope to drive improvement in trial quality and promote greater engagement in trial activity. Do you agree with our trial of the month? Tell us what you think! @ISNeducation Want to run your own trial? ISN-ACT Clinical Trials Toolkit www.theisn.org/isn-act-toolkit Would you like to write your own reviews? Join the GTF team. Contact us at research@theisn.org R A BP BO CD CR B Page 2 of 4 that reduced temperatures should not be routinely employed to avoid hypotension, cardiovascular events and hospitalizations in hemodialysis patients. The use of a set dialysate temperature may be more comfortable for patients and may simplify set-up processes for busy dialysis nurses.
ISN Academy: Diabetes
Dapagliflozin decreases an early kidney-risk marker among people with diabetes and microalbuminuria
Dapagliflozin improves the urinary proteomic kidney-risk classifier CKD273 in type 2 diabetes with albuminuria: a randomized clinical trial
Curovic et al., Diabetes Care (2022).
Summary: This double-blind crossover trial randomized 40 patients with diabetes to receive dapagliflozin 10 mg/day or placebo to investigate the influence of treatment on the urinary proteomic classifier CKD273 score after 12 weeks of drug administration. According to previous trials, urinary proteomic patterns can be used to distinguish high-risk patients with high specificity and sensitivity in the very early stages of disease. Analysis of the CKD273 score, based on 273 urinary peptides, has been identified as an early marker of unfavorable outcomes in normoalbuminuric patients with diabetes. In the current study, participants had microalbuminuria and eGFR ≥45 ml/min/m2 and were receiving renin-angiotensin-aldosterone inhibition. The mean eGFR was 89ml/min/1.73m2 . Treatment with dapagliflozin was associated with a significant lowering of the CKD273 score compared with placebo (-0.221; 95% CI -0.356, – 0.087; P = 0.002), and those receiving dapagliflozin were less likely to have a high-risk CKD273 score after 12 weeks (44% vs 75%, p=0.021). Eight patients were not included in the final analysis due to protocol violation and proteomic analysis failure. Overall treatment adherence was >80% for both groups.
Comment: The use of SGLT2-inhibitors is associated with kidney fibrosis retardation in mouse models butsupporting evidence in humans isstill lacking. Considering the risks of performing kidney biopsies in normo- or microalbuminuric diabetic patients, the utility of indirect markers of kidney damage, including reductions in proteinuria and changes in urinary proteomic patterns, is very high. According to the results of this trial, dapagliflozin results in a significant reduction of urinary proteomic classifier CKD273 score, providing further supporting evidence for the nephroprotective effects of SGLT2i even in early stages of diabetic kidney disease.
ISN Academy: Transplant
Immunogenicity of additional dose of COVID-19 vaccine may not be different between viral vector or mRNA vaccines
An additional dose of viral vector COVID-19 vaccine and mRNA COVID-19 vaccine in kidney transplant recipients: A randomized controlled trial (CVIM 4 study)
Bruminhent et al. Am J Transplant (2022)..
Summary: Eighty-five kidney transplant recipients who had received primary COVID-19 vaccination with two inactivated viral vector vaccines were randomized to receive a third vaccine dose with either a messenger ribonucleic acid (mRNA) vaccine (M group; BNT162b2/Pfizer-BioNTech or mRNA-1273/Moderna; n=43) or a viral vector vaccine (V group; ChAdOx1 nCoV-19/AstraZeneca; n=42). All included patients were at least 30 days post-transplant with stable allograft function. A total of 52 (68%) participants achieved seroconversion. There was no significant difference in the seroconversion rate between the M and V groups on intention-to-treat analysis (70% vs. 65%, p=0.63) at two weeks after the additional dose, although the signal of higher rates of seroconversion with mMRA vaccination was more pronounced on per-protocol analysis (70% vs 61%, p=0.44). Of the 49 participants who were previously seronegative, 24 (49%; 14 and 10 patients in the V and M groups, respectively) seroconverted. The rate of S1-specific T cell and RBD-specific B cell responses were comparable between two groups. Those who had undergone transplant more than a year prior and those with a higher absolute lymphocyte count had a significantly greater chance of seroconversion after receiving an additional vaccine dose; similarly, a non-mycophenolic acidbased regimen was a favourable factor for seroconversion. Overall safety findings were reassuring, however, pain at the injection site was reported more often in the M group.
Comment: Solid organ transplant recipients are considered to be at greater risk for developing severe COVID-19 infection, which carries a higher risk of morbidity and mortality. A standard two-dose COVID-19 vaccine regimen was noted to have suboptimal immunogenicity across vaccine platforms. Previous studies have shown that inactivated COVID-19 viral-vector vaccines produce relatively weak immune responses in kidney transplant recipients compared with mRNA-based vaccines. This study demonstrated that an additional dose of mRNA vaccine did not perform significantly better than the viral vector vaccine in kidney transplant recipients previously vaccinated with a standard regimen. Limitations of the study include that a higher proportion of participants receiving the mRNA vaccine were within their first year of transplantation and/or had received interleukin-2 receptor antagonists for induction therapy, and this group also had a lower mean level of COVID-19 antibodies at baseline, which may all reduce apparent vaccine efficacy in this treatment arm. Longer term immunogenicity and safety were not assessed. The loss to follow-up and treatment crossover may have led to under-powering of the per-protocol analysis and reduces confidence in the results. The study nonetheless supports that both COVID-19 vaccine types can be offered to kidney transplant recipients, and induces immunity to some extent.
ISN Academy: Dialysis
Insomnia and mood improved by group cognitive behavior therapy in hemodialysis patients
Cognitive behavioural group therapy for insomnia (CBGT-I) in patients undergoing haemodialysis: randomized clinical trial
Shareh et al. Behav Cogn Psychother (2022)..
Summary: In this single center, double-blind study, 34 adult patients with CKD stage 4-5 (without kidney replacement therapy), uncontrolled hypertension (systolic BP>140 mmHg and/or diastolic BP>90 mmHg), volume overload and loop diuretic use for ≥3 months, were given bumetanide 3 mg daily and were randomized to either combination therapy with chlorthalidone 50 mg or to placebo. Volume overload was diagnosed by bioelectrical impedance analysis and defined as fluid volume above the 90th percentile of a presumed healthy reference population. The median total body fluid was similar at 32.7L for the experimental group compared to 33.1 for the control group. Between baseline and day 7, the combination therapy resulted in a significantly greater reduction in total body water (-2.5L vs -0.59 L in the control group, p=0.003) and in extracellular water (-1.58 vs -0.43L, p=0.028). By day 30, extracellular water was markedly lower with the combination treatment (-3.05 vs -0.15L, p<0.001), and there was also a significantly more prominent decrease in systolic BP (-26.1 vs -10 mmHg p=0.028) and diastolic BP (-13.5 vs. 3.4 mmHg, p =0.018). The most common adverse event was the rise in serum creatinine >0.3 mg/dL that occurred in 11 patients in the chlorthalidone group and in 4 patients in the placebo group (p=0.013). However, a doubling of serum creatinine levels was not observed in any of these cases.
Comment: Volume overload and poorly controlled hypertension are among the most common problems in people with advanced CKD stages. A combination of loop and thiazide diuretics has been successfully used for decades in patients with heart failure and nephrotic syndrome, however, the efficacy of this regimen in CKD stages 4-5 has not been thoroughly investigated. HEBE-CKD trial showed that the addition of chlorthalidone dramatically increases short-term efficacy of the loop diuretic in the treatment of fluid overload, assessing by bioimpedance analysis, and hypertension in this category of patients. However, the long-term efficacy and safety of thiazide diuretics in this setting should be tested in further trials.
ISN Academy: Dialysis
Over a 2-year period, vitamin K2 supplementation did not conclusively preserve bone density in dialysis patients
Vitamin K supplementation and bone mineral density in dialysis: results of the double-blind, randomized, placebo-controlled RenaKvit trial
Levy-Schousboe et al. Nephrol Dial Transplant (2022)..
Summary: This double-blind, multi-center trial enrolled 123 adult patients on maintenance hemo- or peritoneal dialysis. To assess whether a daily supplement of vitamin K2 could counteract bone disease in dialysis patients, participants were randomized to receive either Vitamin K2 supplementation as menaquinone-7 (MK-7) at a fixed dose of 360µg or placebo for 2 years. To be eligible, participants needed to not be treated with vitamin K supplements, vitamin K antagonists, recombinant parathyroid hormones or anti-osteoporotic drugs. The primary outcome, assessed by Dual-energy X-ray Absorptiometry (DXA), was the change in bone mineral density (BMD) of the 1/3 distal radius (a marker of fracture risk in dialysis patients). There was a 47% study dropout by 2 years, balanced between treatment arms. With vitamin K versus placebo, after 2 years, there was a greater relative decrease in BMD of the 1/3 distal radius (-0.041g/cm2 vs -0.018g/cm2 , p=0.004) and a greater relative increase in BMD of the lumbar spine (0.022g/cm2 vs -0.028g/cm2 , P=0.005). There were no other significant changes in BMD or biomarkers of mineral and bone disease turnover. Supplementation significantly improved biomarkers of vitamin K status. Therapy was well tolerated with no concerning safety signals.
Comment: In the elderly general population, vitamin K supplementation has been positively associated with BMD, but this has not previously been investigated in dialysis patients in an RCT. In this study, supplementation with vitamin K had a variable effect on BMD by site. No previous vitamin K trials in other populations demonstrated a relative worsening of BMD at any skeletal site. The authors suggest that the high drop-out rate may have led to a type 1 statistical error to explain these conflicting results. Further, lumbar spine osteoarthritis and intake of phosphate binders can falsely increase BMD results on DXA, and residual peritoneal dialysate may also affect BMD results, although the proportion of patients receiving phosphate binders and peritoneal dialysis were balanced between groups. Larger RCTs with different dosing regimens and longer follow-up periods are needed to further explore this treatment approach. Additionally, it may be necessary to examine bone fracture as the primary outcome, since an observational study (Booth et al Am J Clin Nutr, 2000) found an association between vitamin K intake and fracture among dialysis patients, without an apparent effect on BMD, suggesting that vitamin K could result in benefits to bone health through mechanisms other than BMD.
Edited by Daniel O’Hara, Michele Provenzano, and Anastasiia Zykova